Retinal Diseases Treatment In Mumbai
Retinal diseases encompass a wide range of conditions that affect the retina, the light-sensitive tissue at the back of the eye that is crucial for vision. These diseases can lead to varying degrees of vision loss, and in some cases, blindness.
If you notice vision problems or symptoms of retinal diseases, it’s important to consult an eye care professional for proper diagnosis and treatment options.
Types of Retinal Diseases
Here’s an overview of some of the most common retinal diseases:
Age-Related Macular Degeneration
Overview: AMD is a leading cause of vision loss in individuals over 50 years old. It affects the macula, the central part of the retina responsible for sharp, detailed vision.
Types:
- Dry AMD: The more common form, characterized by the gradual breakdown of the macula.
- Wet AMD: A more severe form where abnormal blood vessels grow beneath the retina and leak fluid or blood, causing rapid vision loss.
Symptoms: Blurred or distorted central vision, difficulty recognizing faces, and seeing straight lines as wavy.
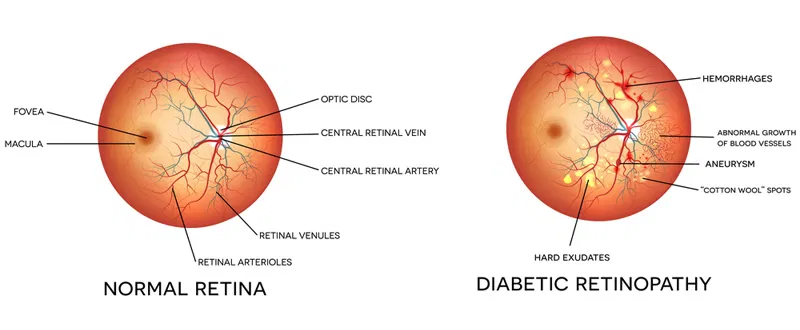
Diabetic Retinopathy
Overview: A complication of diabetes, this condition occurs when high blood sugar levels damage the blood vessels in the retina.
Stages:
- Non-Proliferative Diabetic Retinopathy (NPDR): Early stage, characterized by the swelling of blood vessels and leakage of fluid.
- Proliferative Diabetic Retinopathy (PDR): Later stage, where new, abnormal blood vessels grow, potentially leading to bleeding and scarring.
Symptoms: Blurry vision, floaters, or sudden vision loss in advanced stages.
Management: Strict blood sugar control, laser treatment, or injections to prevent progression.
Retinal Detachment
Overview: A serious condition where the retina separates from its underlying support tissue. This disrupts its ability to send visual signals to the brain.
Causes: Often caused by trauma, advanced diabetic retinopathy, or age-related changes like vitreous detachment.
Symptoms: Sudden flashes of light, a curtain or shadow over vision, and an increase in floaters.
Treatment: Surgical intervention is typically required to reattach the retina.
Retinitis Pigmentosa
Diabetic Macular Edema
Retinitis Pigmentosa
Retinal Vein Occlusion
Macular Hole
Retinopathy of Prematurity
Choroidal Neovascularization
Toxoplasmic Retinitis
Inherited Retinal Diseases
Causes of Retinal Diseases
Retinal diseases can arise from a variety of causes, ranging from genetic factors to environmental influences and systemic health conditions. Here’s an overview of the primary causes of retinal diseases:
Genetics: Many retinal diseases are genetic in origin, passed down through families.
Age-Related Macular Degeneration (AMD): The most common cause of vision loss in older adults. With aging, the macula (the central part of the retina) begins to deteriorate.
Diabetic Retinopathy: Diabetes, particularly when poorly controlled, can damage the small blood vessels in the retina.
Hypertensive Retinopathy: Chronic high blood pressure can damage the blood vessels in the retina, leading to retinal hemorrhages, swelling, and narrowing of blood vessels.
Trauma or Injury: Physical trauma or injury to the eye, such as a blow to the head or eye, can cause the retina to detach.
Infections: Caused by the Toxoplasma gondii parasite, often acquired through contact with infected cat feces or undercooked meat.
Inflammatory Diseases, Blood Flow Issues, Tumors and Growths, Vitamin Deficiencies, Autoimmune Disorders, Smoking and Environmental Factors, Vitreous Changes, Medications or Other Health Conditions
Symptoms of Retinal Diseases
Symptoms of retinal diseases can vary widely depending on the specific condition, its severity, & the part of the retina affected. Early detection of retinal disease symptoms is crucial for effective treatment & preventing permanent damage to vision.
Blurred or Distorted Vision
Blurring or a decrease in the sharpness of central vision, often making it difficult to read, recognize faces, or see fine details.
Loss of Central Vision
Difficulty seeing objects clearly in the center of the visual field, leading to problems with reading, driving, and other tasks requiring detailed vision.
Floaters
Tiny spots, strands, or cobweb-like shapes that appear to float across the field of vision. They are typically more noticeable when looking at a bright background
Flashes of Light
Seeing flashes or streaks of light, especially in peripheral vision, often described as “lightning streaks.” This can occur when the vitreous gel inside the eye pulls away from the retina.
Distorted or Wavy Vision
Straight lines may appear wavy or bent. This is often a sign of macular involvement, particularly when abnormal fluid buildup or scar tissue affects the macula.
Sudden Vision Loss or Blind Spots
A sudden loss of vision in one eye, often described as a “blackout” or “curtain” covering part of the visual field.
Treatment
Treatment varies depending on the disease, but common options include:
Laser Therapy: Used for conditions like diabetic retinopathy and retinal vein occlusion to reduce swelling or abnormal blood vessel growth.
Injections: Anti-VEGF drugs (like Lucentis, Eylea) are commonly used for conditions such as wet AMD and diabetic macular edema.
Surgical Intervention: Retinal detachment, macular holes, and certain types of diabetic retinopathy may require surgery.
Steroids and Immunosuppressants: Used for conditions like uveitis.
Prevention
Regular eye exams: Especially for those at high risk (e.g., diabetics, people with a family history of retinal diseases, or the elderly).
Blood sugar control: For diabetes management, to prevent diabetic retinopathy.
Quit smoking: Smoking increases the risk of age-related macular degeneration and other retinal diseases.
Get Advanced Retinal Disease Treatment in Mumbai
If you experience symptoms of Retinal Diseases, it’s important to consult an eye care professional for a proper diagnosis and treatment plan.
Why Choose Sahu Eye Hospital for Retinal Diseases Treatment in Mumbai?
Choosing Sahu Eye Hospital for retinal diseases means you’ll benefit from skilled surgeons, advanced technology, and personalized care that puts your needs and comfort first. With a focus on achieving the best possible outcomes and a commitment to making the process as smooth as possible, we provide a comprehensive approach to help you regain clear, vibrant vision.
- Expertise and Experience
- State-of-the-Art Technology
- Personalized Care
- Exceptional Patient Care
- High Success Rate
- Advanced Diagnostic Tools
- Comprehensive Aftercare
- Affordable Care
- Post-Surgery Monitoring
- Cutting-Edge Intraocular Lenses
- Patient Education
- Convenient Locations
FAQs
What is Diabetic Retinopathy?
Your eye has a part called the Retina. It is the most important part of the eye and is the part on which your vision depends the most. In patients who have Diabetes, the blood vessels in the Retina get affected. Patients can develop swelling in the central part of the Retina called the Macula and in late stages even develop bleeding in the eye. These changes are called ‘Diabetic Retinopathy’
I have Diabetes, when should I get my eyes checked?
Ideally, the first time you are diagnosed with Diabetes, a baseline Retina evaluation should be done. This is because Diabetes might have been present for many years and not been detected. Then onwards, the follow up depends on which stage of Diabetic Retinopathy is present. However, in the best scenario also, an annual Retina check is mandatory.
What if my vision is affected because of Diabetic Retinopathy? What is the further line of treatment?
As part of treatment, good control of your Diabetes along with Hypertension, Dyslipidemia if present is mandatory. The treatment depends on whether you have developed Macular edema or Vitreous hemorrhage or both. Treatment options include green laser, injections like Avastin/Lucentis/IVTA and sometimes even surgery.
Will my vision improve or always remain poor?
Vision does improve in most cases but it depends on various factors. It is difficult to generalize and it is best that you discuss with your doctor the visual prognosis in your case.
How often do I need to undergo laser/take injections?
Generally, if the laser is being done for macular edema, 1 sitting is enough. If the laser is being done for Proliferative Diabetic Retinopathy, it depends on the machine being used. If your doctor has a Pattern laser, it can be completed in 2 sittings or else 3 sittings are generally required.
As far as the injections are concerned, it is difficult to generalize, there are patients who become alright following a single injection and there are patients who at times require multiple injections.
I have bleeding in my eye, do I need to undergo surgery immediately?
No, most doctors do laser, wait for a period of a month and stabilization of your overall health before they plan surgery. However, there are certain situations where your doctor may advise surgery immediately. These are Macular tractional detachment or Combined Retinal detachment.
I have undergone surgery for bleeding, what precautions do I need to take?
Apart from the general precautions following any general surgery like
Follow the doctor’s instructions as far as the medicines are concerned.
Avoid head bath for at least 10 days
Avoid rubbing, squeezing your eyes
Avoid putting water into your eyes
Avoid using soiled hand kerchief or any cloth around the eyes
Avoid areas where there is dust
Use dark glasses outside the house for at least 10 days.
You may have to adopt certain positions if gas or oil has been used by the doctor during surgery. Also, you have to keep a strict control of Blood Sugar, Cholesterol and Blood pressure.

