What Is Corneal Diseases?
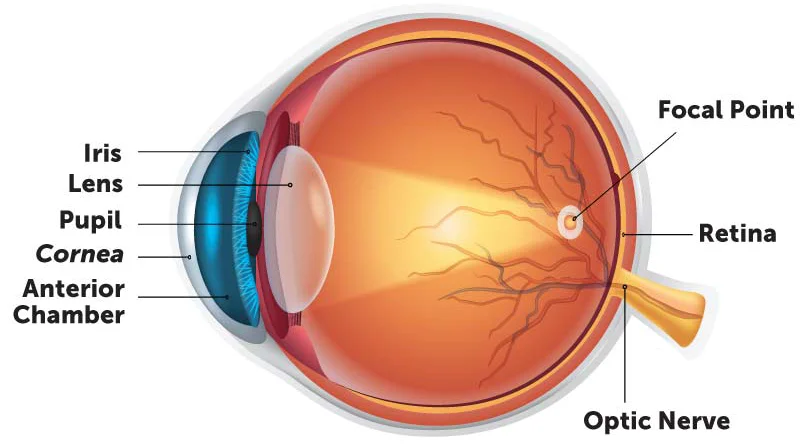
Corneal diseases refer to any conditions that affect the cornea, the transparent, dome-shaped layer at the front of the eye.
The cornea plays a critical role in focusing vision and protecting the inner structures of the eye. When the cornea becomes damaged or diseased, it can lead to various visual problems or even blindness.
If you experience symptoms like sudden vision changes, pain, redness, or sensitivity to light, it’s important to see an eye care professional (optometrist or ophthalmologist) for an accurate diagnosis and appropriate treatment.
Types of Corneal Diseases
Here’s an overview of some of the most common Glaucoma Type:
Congenital/Hereditary
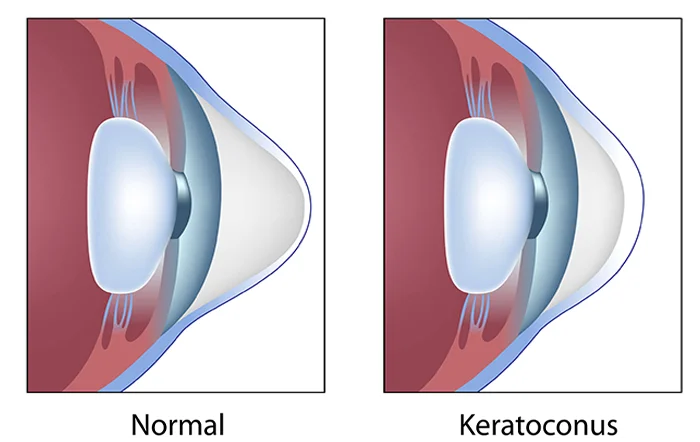
Condition: Keratoconus, Fuchs’ Endothelial Dystrophy, Corneal Dystrophies
Traumatic
Condition: Corneal Abrasions, Lacerations, Chemical Burns
Infectious
Condition: Bacterial Keratitis, Herpes Simplex Virus Keratitis, Fungal Keratitis, Acanthamoeba Keratitis
Degenerative/Non-Infectious
Condition: Bullous Keratopathy, Pterygium, Terrien’s Marginal Degeneration, Pellucid Marginal Degeneration
Edema/Swelling
Condition: Corneal Edema, Bullous Keratopathy
Scarring
Condition: Corneal Opacities (Leucomas)
Neovascularization
Condition: Corneal Neovascularization
Dry Eye Disease
Condition: Keratomalacia, Dry Eye Syndrome
Post-Surgical Complications
Condition: Post-Transplantation Rejection, Corneal Ectasia (from LASIK)
Causes of Corneal Diseases
The causes of corneal diseases can vary widely depending on the specific condition. Below are the main categories of causes for corneal diseases:
Genetic/Hereditary: Keratoconus, Fuchs’ Dystrophy, Corneal Dystrophies
Trauma/Injury: Abrasions, Lacerations, Chemical Burns, UV Exposure
Infections: Bacterial, Viral (Herpes), Fungal, Acanthamoeba
Inflammation/Autoimmune: Allergies, Autoimmune Diseases, Anterior Uveitis
Environmental: UV Exposure, Dry Air, Contact Lenses, Pollution
Other conditions: Degenerative, Nutritional Deficiencies, Systemic Diseases & Post-Surgical
Symptoms of Corneal Diseases
If you experience any combination of the following symptoms, it’s important to seek evaluation by an eye care professional (optometrist or ophthalmologist) to identify the underlying cause:
Painful or gritty sensation
Pain can range from mild irritation to severe, sharp discomfort. It is often caused by inflammation, infection, or injury to the cornea.
Redness and/or swelling
Eye redness often occurs when the cornea is inflamed or when there is increased blood flow to the area in response to irritation or infection.
Cloudy or blurry vision
Blurred, hazy, or distorted vision is one of the most common symptoms of corneal disease.
Increased sensitivity to light
Increased sensitivity to light is common in many corneal diseases. The cornea is essential for focusing light, and inflammation or damage can make the eye more sensitive.
Frequent tearing or discharge
Excessive tearing (epiphora) or a thick, yellow-green discharge may occur in response to infection or irritation of the cornea.
Halos or glare around lights
Disturbances in vision that cause light to appear with halos or glare, particularly at night or in dim light.
Treatment
If you suspect you have a corneal disease, it’s essential to see an ophthalmologist for diagnosis and to discuss the appropriate treatment options. Early detection can often prevent long-term damage and vision loss.
Non-surgical: Artificial tears, anti-inflammatory medications, antibiotics, antivirals, antifungals, and contact lenses (e.g., rigid gas permeable lenses for keratoconus).
Surgical: Corneal cross-linking (for keratoconus), corneal transplant (for Fuchs’ dystrophy, severe scarring, or other advanced conditions), or laser surgery (e.g., for post-surgical ectasia or vision correction).
Prevention
Regular Eye Exams: Early detection of corneal diseases can help prevent vision loss.
Proper Contact Lens Hygiene: To avoid corneal infections, always clean and store contact lenses properly, and avoid over-wearing them.
UV Protection: Protect your eyes from UV rays by wearing sunglasses with UV protection and a hat with a brim.
Avoid Trauma: Be cautious with activities that could cause eye injury, such as sports or working with chemicals.
Get Advanced Corneal Diseases Treatment in Mumbai
If you experience symptoms of Corneal Diseases, it’s important to consult an eye care professional for a proper diagnosis and treatment plan.
Why Choose Sahu Eye Hospital for Corneal Diseases Treatment in Mumbai?
Choosing Sahu Eye Hospital for Corneal Diseases means you’ll benefit from skilled surgeons, advanced technology, and personalized care that puts your needs and comfort first. With a focus on achieving the best possible outcomes and a commitment to making the process as smooth as possible, we provide a comprehensive approach to help you regain clear, vibrant vision.
- Expertise and Experience
- State-of-the-Art Technology
- Personalized Care
- Exceptional Patient Care
- High Success Rate
- Advanced Diagnostic Tools
- Comprehensive Aftercare
- Affordable Care
- Post-Surgery Monitoring
- Cutting-Edge Intraocular Lenses
- Patient Education
- Convenient Locations
FAQs
How are corneal diseases diagnosed?
- Comprehensive eye exam (including visual acuity testing)
- Slit-lamp examination (to inspect the cornea under magnification)
- Tonometry (to measure intraocular pressure)
- Corneal topography (mapping the surface shape and curvature)
- Fluorescein dye test (used to detect scratches, ulcers, or infections)
- Culture and sensitivity tests (for infections)
Can corneal diseases cause permanent vision loss?
Yes, if left untreated or inadequately managed, corneal diseases can lead to permanent vision loss. Conditions like corneal scarring, keratoconus, or corneal ulcers can result in severe visual impairment. Timely diagnosis and appropriate treatment are crucial to preventing irreversible damage.
How can corneal diseases be prevented?
While some corneal diseases are genetic and cannot be prevented, you can reduce the risk of others by:
- Proper contact lens hygiene (cleaning lenses regularly, not wearing them for extended periods)
- Protecting your eyes from UV light (wearing sunglasses or hats with brims)
- Avoiding eye injuries (wearing safety goggles when necessary)
- Managing underlying conditions (like dry eye or diabetes)
- Avoiding smoking (which can contribute to dry eyes and worsen some corneal conditions)
- Regular eye exams to detect early signs of corneal diseases, especially in individuals with a family history of eye conditions
Is keratoconus treatable?
Yes, keratoconus can be treated, although it requires early detection for the best outcomes. Treatment options include:
- Corneal cross-linking: A procedure that strengthens the corneal tissue to slow or halt the progression of the disease.
- Rigid gas permeable (RGP) contact lenses: These lenses help correct vision by providing a smooth surface over the irregularly shaped cornea.
- Corneal transplant: In advanced cases where other treatments are ineffective, a corneal transplant may be required.
What is a corneal transplant?
A corneal transplant (keratoplasty) is a surgical procedure in which a damaged or diseased cornea is replaced with a healthy donor cornea. It is typically done in cases of severe corneal scarring, Fuchs’ dystrophy, or other corneal conditions that cannot be treated with other methods. After a transplant, patients may need to take immunosuppressive drugs to prevent rejection of the donor tissue.
Can corneal diseases be linked to other health conditions?
Yes, several systemic conditions can impact corneal health:
- Diabetes can lead to corneal neuropathy, which can affect healing and increase the risk of infection.
- Autoimmune diseases (like rheumatoid arthritis and Sjogren’s syndrome) can cause dry eyes and inflammation, which may lead to corneal damage.
- Herpes simplex virus (HSV) can cause herpes keratitis, leading to recurrent corneal ulcers and scarring.
Is it safe to wear contact lenses with corneal disease?
It depends on the type and severity of the corneal disease. For some conditions, such as keratoconus, special rigid gas permeable (RGP) contact lenses may be recommended to help correct vision. However, contact lenses may not be safe for conditions involving active infections, severe corneal ulcers, or severe dry eyes. Always consult an eye care professional before wearing contact lenses if you have a corneal disease.
What is corneal cross-linking, and when is it used?
Corneal cross-linking is a treatment used to strengthen the cornea by using ultraviolet light and a photosensitizing agent (riboflavin). It is primarily used to treat keratoconus and can help prevent the progression of the disease by stabilizing the corneal tissue. This procedure is most effective in the early stages of keratoconus.
Can I prevent corneal scarring after an eye injury or infection?
Prompt and appropriate treatment of eye injuries and infections can help prevent corneal scarring. If you experience an injury or infection, seeking medical attention immediately is important to minimize the risk of permanent scarring. For infections, following prescribed treatments (e.g., antibiotics or antivirals) is critical in reducing the risk of damage to the cornea.
How do I know if I have a corneal disease?
If you experience any of the following symptoms, you may have a corneal disease:
- Blurry vision, halos, or glare around lights
- Eye pain, irritation, or discomfort
- Redness or swelling in the eye
- Sensitivity to light
- Tearing or discharge from the eye
- A foreign body sensation

